How the expansion of telehealth and the waving of HIPAA requirements is helping practices avoid patient cancellations due to the COVID-19 virus
The Centers for Medicare & Medicaid Services (CMS), The Health and Human Services Department (HHS), as well as other health related federal agencies, have continued to waive requirements, or expand services and benefits in an effort to help contain the COVID-19 virus.
In a press release on March 17, 2020, CMS stated that it was broadening access to telehealth services, as well as “not imposing penalties for noncompliance with regulatory requirements under the HIPAA Rules against covered healthcare providers in connection with the good faith provision of telehealth during the COVID-19 nationwide public health emergency.” Prior to March 17, 2020, a physician who communicated with a patient over their cell phone, for example, could face fines and penalties for violating HIPAA requirements that required the physician to ensure that the data seen on his or her cell phone from the patient was encrypted. Now, with this waiver, a physician can communicate with a patient over their cell phone if they make a “good faith effort” to keep the information as confidential as possible.
Since physicians will want to know now what they can and cannot do as it pertains to telehealth, HIPAA, and the COVID-19 virus, this article will discuss the expansion of telehealth with the 1135 waiver; types of virtual services that will temporarily be allowed; and how the waived HIPAA requirements affect the telehealth expansion.
EXPANSION OF TELEHEALTH WITH 1135 WAIVER
Thanks to this waiver, CMS will now pay for office, hospital, and other “visits furnished via telehealth across the country, including in patient’s places of residence.” Basically, instead of your patients cancelling appointments because they don’t want to come into your office for fear of contracting the COVID-19 virus, you don’t have to necessarily reschedule them. You can now use telehealth to conduct a normal office visit with the patient without the patient ever leaving their home. CMS has opened this ability up to a wide range of medical providers including physicians, nurse practitioners and physician assistants so that they can offer these services to their patients.
Before this waiver, CMS could only pay for telehealth services on a limited basis. Basically, the patient had to be in a rural area and unable to obtain medical attention without driving a long distance. With the waiver, patients can now be seen for common office visits, mental health counseling and preventive health screenings. HHS has even gone as far to say that they are allowing covered entities, i.e., physicians, to use “non-public facing audio or video communication products during the COVID-19 nationwide public health emergency.” HHS stated that this ability “applies to telehealth provided for any reason, regardless of whether the telehealth service is related to the diagnosis and treatment of health conditions related to COVID-19.” For example, a physician may now provide telehealth services in the exercise of their medical professional judgement to assess or treat any medical condition, whether it is related to COVID-19 or not, such as sprained ankle, dental consultation, psychological evaluations, or other conditions. CMS noted that “These visits are considered the same as in-person visits and are paid at the same rates as regular, in-person visits.”
The telehealth expansion and HIPAA waivers may apply to patients you see that are not on Medicare, or a Medicare Advantage Plan, but have insurance nonetheless with a private payer like Anthem, United Healthcare, Cigna, or VSP. Contact your private payer representative to determine if the private payer insurance will cover the telehealth service for non-COVID-19 related services, as well as for COVID-19 services.
TYPES OF VIRTUAL SERVICES
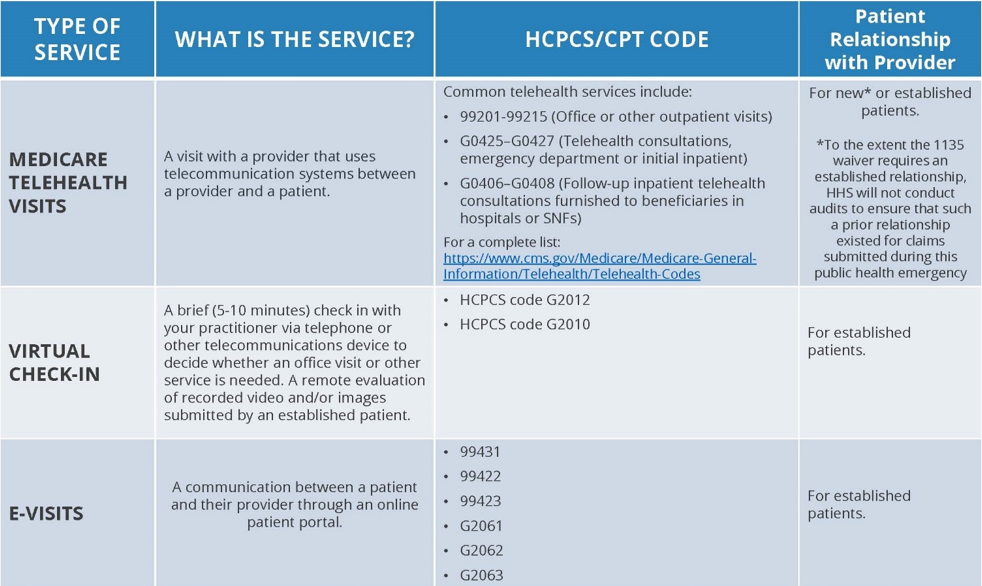
CMS has listed three types of virtual services that can be performed by a medical practice through telehealth expansion and the requirements each has in order for the physician to get reimbursed for his or her services. The three are: Medicare Telehealth Visits, Virtual Check-Ins, and E-Visits.
Medicare Telehealth Visits:
Under these visits, the provider must use an interactive audio and video telecommunications system that permits real-time communication between the distant site and the patient. HHS stated that “to the extent the waiver requires that the patient have a prior established relationship with a particular practitioner, HHS will not conduct audits to ensure that such a prior relationship existed for claims submitted during this public health emergency.” So, if a patient calls your office and wants to be seen via telehealth, and they were not a patient of yours prior to the call, you can see them, and HHS wouldn’t audit you to determine if there was a prior relationship.
Virtual Check-Ins:
According to CMS, in all areas, not just rural, established Medicare patients of a physician can have a brief communication via the phone or text with the physician and Medicare will pay for it. This allows these patients to avoid unnecessary trips to their physician’s office. The patient must have already seen the physician prior to the use of this service, and the communication cannot be related to a medical visit that they had with the physician in the last 7 days. The patient must consent to receiving these Virtual Check-In services from the physician.
Again, if your patients are calling and cancelling and they can conduct these virtual check-ins with your practice, you would not have to cancel and or reschedule their appointment. It is imperative that they already be patients of yours prior to doing this however, because CMS will still NOT pay for new patient visits conducted through this system.
E-Visits:
In all types of locations including the patient’s home, and in all areas (not just rural), established Medicare patients may have non-face-to-face patient-initiated communications with their doctors without going to the doctor’s office by using online patient portals, and still give you the right to bill for the service. The patient must be the one to initiate this service; however, you can educate your patients that this is now available to them should they chose to keep their appointment, but not come into the office.
To help with explaining how this all works, CMS has developed the following chart:
Summary of Medicare Telemedicine Services:
*Again, this may be allowed by the patient’s private payer insurance, but check with your private payer rep before seeing patients via telehealth for non-related COVID-19 services.
HIPAA WAIVER
HHS has stated that, “the HHS Office for Civil Rights (OCR) will exercise enforcement discretion and waive penalties for HIPAA violations against health care providers that serve patients in good faith through everyday communications technologies, such as FaceTime or Skype, during the COVID-19 nationwide public health emergency.” Therefore, physicians can communicate now with their patients via telehealth through remote communication systems like Skype and Facetime, without the worry of being audited and fined for violating HIPAA Privacy Rule requirements. Waiving this makes it so much easier for you to see your patients, keep up with their healthcare, and hopefully allow you to not have to cancel and reschedule so many patients.
CONCLUSION
While all of us may be self-quarantining in order to slow and/or prevent the virus from spreading, medical care of patients must continue. With HHS and CMS waiving HIPAA requirements and expanding telehealth services, patients can now, temporarily, continue to see their physicians without ever leaving their homes. Physicians can rest easy knowing that they will not get fined or penalized for using Skype, Facetime, or other audio and video enabled systems to meet with and discuss their patients’ needs. Make sure that you are billing these services correctly to CMS, and that all of this applies only to Medicare, Medicaid, Tricare, or Medicare Advantage Plans, and not necessarily private payers. Check with your private payer representatives, like United Healthcare, Anthem, Aetna, or others as to whether they will be allowing these services temporarily for your patients or not. Just because the COVID-19 virus has caused a huge disruption in our everyday lives, does not mean that your patients medical needs have stopped. These waivers of requirements and expansion of services goes along way to helping you continue to provide top-quality medical services during this time.
